What Does Foot Fungus Look Like?
Have you ever wondered what foot fungus actually looks like? Perhaps you’ve heard about it or even experienced it yourself. Well, in this article, we will explore the appearance of foot fungus, shedding light on its distinctive characteristics and providing you with valuable insights to help you identify and treat this common condition. So, if you’re curious about knowing more about foot fungus and its visual manifestations, keep on reading!

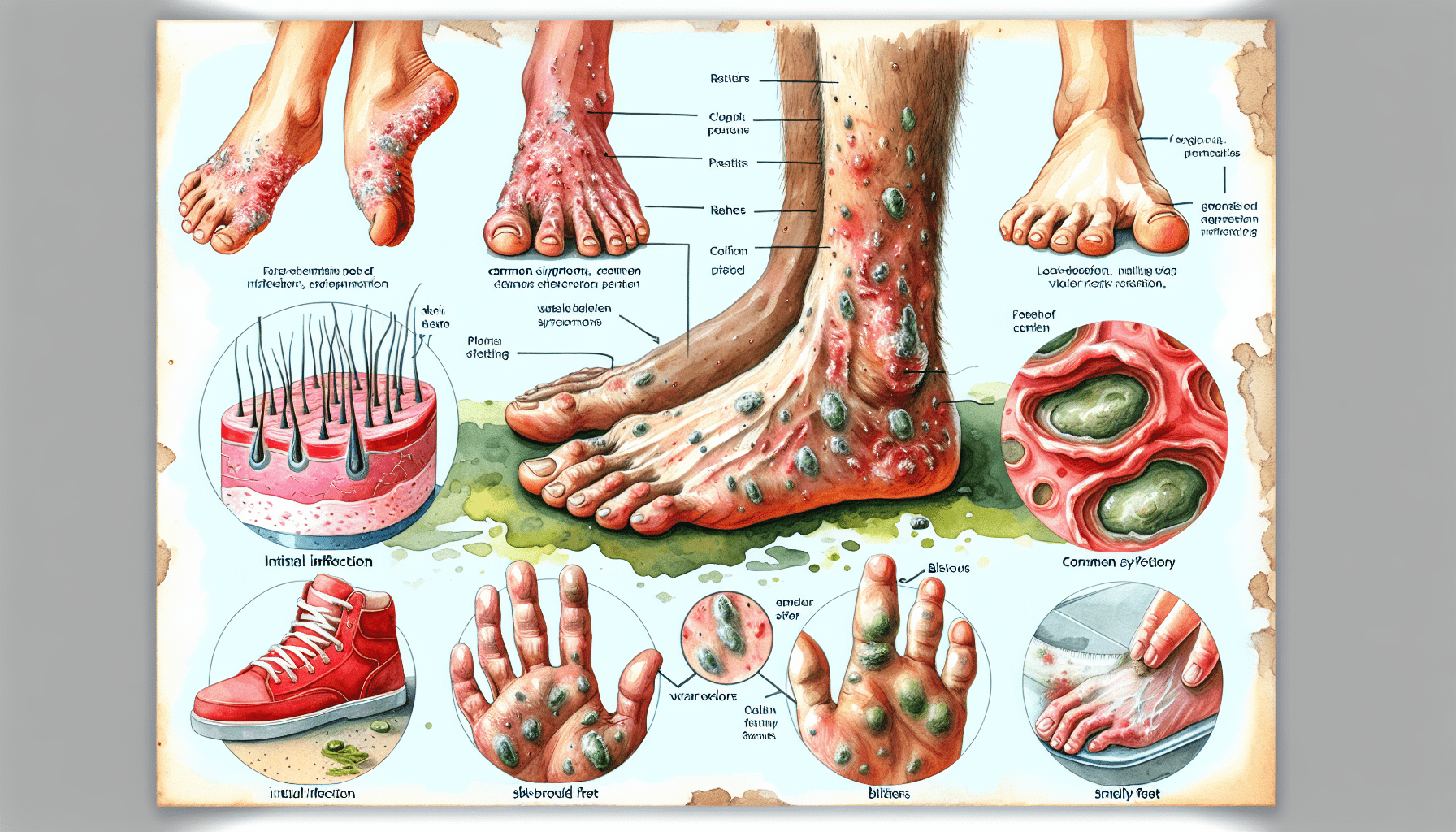
Appearance
Color
When it comes to foot fungus, the appearance can vary depending on the particular type of fungus. One common characteristic is a change in color. Fungal infections can cause the skin or toenails to become discolored. In the case of athlete’s foot, the skin may appear red and inflamed. Toenail fungus, on the other hand, can cause the nails to turn yellow or even brown in some cases.
Texture
Another aspect of foot fungus to take note of is the texture. Fungal infections can lead to changes in the texture of the affected area. For example, athlete’s foot may cause the skin to become scaly and rough. Toenail fungus can make the nails thickened and brittle, giving them an uneven or crumbly texture.
Shape
Foot fungus can also impact the shape of the affected area. In the case of athlete’s foot, the skin may appear cracked and peeling, which can be uncomfortable and unsightly. Toenail fungus can cause the nails to become distorted, with an irregular shape. It’s important to pay attention to any changes in the shape of your feet or nails, as these could be signs of a fungal infection.
Symptoms
Itching
One of the most common symptoms of foot fungus is itching. You may notice an intense, persistent itch on the affected area. This itching can be especially bothersome in between the toes in the case of athlete’s foot. The urge to scratch can be difficult to resist, but it’s important to avoid scratching as it can further irritate the skin and lead to complications.
Burning sensation
Along with itching, a burning sensation is another symptom that may accompany foot fungus. The affected area can feel hot or like it’s burning, which can be uncomfortable and even painful at times. This burning sensation is often experienced by individuals with athlete’s foot or jock itch.
Scaling
Scaling refers to the formation of dry, flaky skin on the affected area. This can occur in various types of foot fungus, including athlete’s foot and ringworm. These flakes of skin may appear white or gray and can be easily seen when the affected area is examined closely.
Peeling skin
In some cases, foot fungus can cause the skin to peel. This can create a layer of dead skin that may come off in small pieces or even larger chunks. Peeling skin is often seen in athlete’s foot, especially between the toes.
Redness
Redness is a common symptom of foot fungus. The affected area may appear reddened and inflamed. This can be especially noticeable in cases of athlete’s foot or jock itch, where the skin can become quite irritated and sensitive.
Blistering
Certain types of foot fungus, such as athlete’s foot, can lead to the formation of blisters. These blisters may be small and filled with fluid. They can be painful and may even burst, exposing raw skin underneath.
Cracking skin
Cracking skin is another symptom that can occur with foot fungus, particularly in athlete’s foot. The skin may crack and develop painful fissures, making it difficult and uncomfortable to walk or engage in regular activities.
Pain
Foot fungus can also cause pain in the affected area. This pain can range from mild discomfort to sharp, stabbing sensations. It can make it challenging to wear certain types of shoes or engage in physical activities.
Unpleasant odor
Another symptom of foot fungus is an unpleasant odor. Fungal infections can produce a distinct smell that is often described as sour or musty. This odor is particularly common in cases of athlete’s foot and can be bothersome and embarrassing.
Types of Foot Fungus
Athlete’s Foot
Athlete’s foot, also known as tinea pedis, is a common type of foot fungus. It typically affects the skin between the toes and the soles of the feet. Athlete’s foot is contagious and can be spread through direct contact with an infected person or by coming into contact with contaminated surfaces.
Toenail Fungus
Toenail fungus, medically known as onychomycosis, is a fungal infection that affects the nails. It commonly starts at the tip of the toenail and gradually spreads deeper into the nail bed. Toenail fungus can cause the nails to become thickened, discolored, and brittle.
Jock Itch
Jock itch, or tinea cruris, is a type of fungal infection that affects the groin area. It is characterized by redness, itching, and a distinct rash with raised edges. Jock itch commonly occurs in athletes or individuals who sweat heavily in the groin region.
Ringworm
Contrary to its name, ringworm is not caused by a worm but is a fungal infection that can affect various parts of the body, including the feet. It presents as circular patches of red, scaly skin with a clear center and raised edges. Foot ringworm can cause itching and discomfort.
Appearance of Athlete’s Foot
Red and scaly skin
One of the primary characteristics of athlete’s foot is the presence of red and scaly skin. The affected area may appear inflamed and have a rough texture due to the scaling skin.
Itchy and burning sensation
Athlete’s foot is notorious for causing intense itching and a burning sensation. The urge to scratch can be almost unbearable, and the constant itchiness can be highly disruptive to daily activities.
Blisters and ulcers
In severe cases, athlete’s foot can lead to the formation of blisters. These blisters may contain clear fluid and can be painful. If left untreated, the blisters can burst and form ulcers, which can increase the risk of secondary infections.
Cracked and peeling skin
Athlete’s foot can cause the skin on the affected area to crack and peel. This can create an uncomfortable and unsightly appearance. The peeling skin may come off in small flakes or larger pieces, contributing to the spread of the infection if not properly managed.
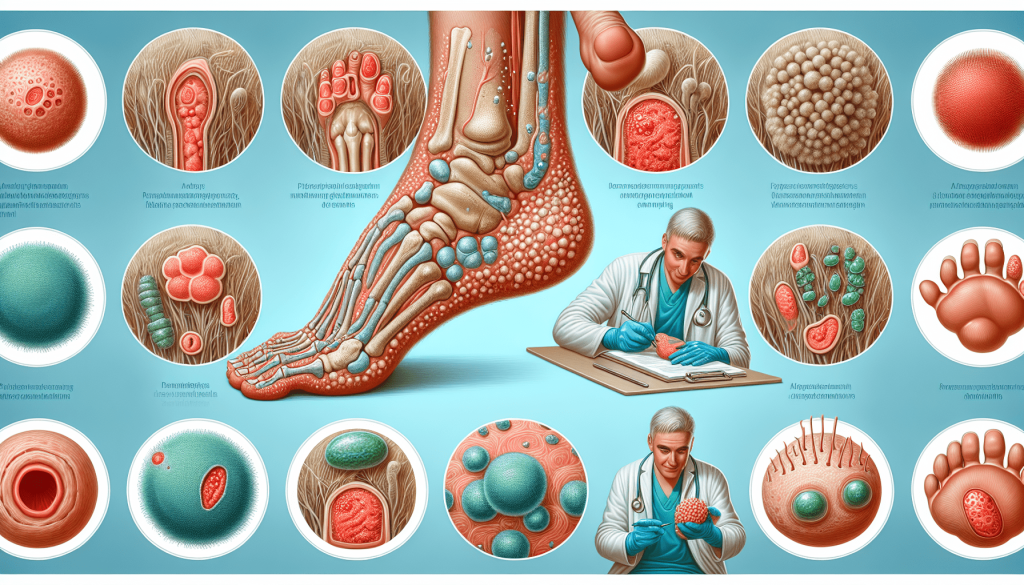
Appearance of Toenail Fungus
Thickened toenails
Toenail fungus often causes the nails to become thickened. The affected nails can appear noticeably thicker than usual and may feel heavier. In severe cases, the thickening can cause discomfort and difficulty in wearing narrow or tight-fitting shoes.
Yellow or brown discoloration
Discoloration is a hallmark sign of toenail fungus. The nails may take on a yellow or brown hue, with noticeable changes in color from the nail bed to the tip. The discoloration can intensify as the infection progresses.
Brittle or crumbly nails
Nails affected by fungus tend to become brittle and crumbly. They may easily break or split, making them more susceptible to further damage. This can pose a challenge when trying to maintain proper nail hygiene.
Distorted nail shape
Toenail fungus can cause the nails to become misshapen or distorted. The infected nails may curve or develop ridges, making them appear abnormal and irregular. In severe cases, the nail may even detach from the nail bed.
Appearance of Jock Itch
Red and itchy groin area
Jock itch primarily affects the groin area, causing redness and itchiness. The skin in the affected area may appear reddened and may feel warm to the touch. The constant itching can be highly uncomfortable and may worsen with moisture or friction.
Inflammation and soreness
Along with redness and itchiness, jock itch can cause inflammation and soreness. The affected area may be swollen and tender. This can make activities such as exercising or wearing tight-fitting undergarments particularly uncomfortable.
Rash with raised edges
A distinct characteristic of jock itch is the presence of a rash with raised edges. The rash often forms a circular or oval shape, spreading outwards from the central area. The raised edges can be itchy and may contribute to further skin irritation.
Flaking or peeling skin
Jock itch can lead to flaking or peeling of the skin in the groin area. The affected skin may become dry and start to peel off in small flakes. This can worsen the itching and make the skin feel even more sensitive.
Appearance of Ringworm
Red, itchy, and scaly patches
Ringworm can cause red, itchy, and scaly patches on the skin. These patches may have a raised appearance and can be round or oval in shape. The affected skin may feel rough and may appear inflamed.

Ring-shaped rash
As the name suggests, ringworm often manifests as a ring-shaped rash. The outer edges of the rash are typically reddened and slightly raised, while the center may appear clearer or less inflamed. The circular shape of the rash is a distinctive feature of ringworm.
Clear center with raised edges
The rash caused by ringworm often has a clear center, surrounded by raised and reddened edges. This gives the appearance of a ring or circle on the skin. The clear center can sometimes make the rash resemble a patch of healthy skin, leading to confusion or delayed diagnosis.
Causes
Fungal infection
The primary cause of foot fungus is a fungal infection. Fungi, such as dermatophytes, thrive in warm and moist environments, making the feet an ideal breeding ground. These fungi can invade the skin or nails, leading to various types of foot fungus.
Poor foot hygiene
Lack of proper foot hygiene can contribute to the development of foot fungus. Failing to keep the feet clean and dry provides an environment conducive to fungal growth. Regularly washing and thoroughly drying the feet can help prevent fungal infections.
Walking barefoot in public areas
Walking barefoot in public areas, such as locker rooms or communal showers, increases the risk of coming into contact with fungi. The fungi can then cling to the skin or nails, leading to infection. It is advisable to wear protective footwear, such as flip-flops, in such environments.
Sharing personal items
Sharing personal items, particularly socks or shoes, can facilitate the spread of foot fungus. Fungi can survive on these items and be transferred from one person to another. It is essential to avoid sharing footwear or socks to minimize the risk of infection.
Sweaty feet
Excessive sweating, particularly on the feet, can create a moist environment that is favorable for fungal growth. Individuals with sweaty feet are more susceptible to developing foot fungus. Maintaining good foot hygiene and wearing breathable footwear can help manage sweat and prevent fungal infections.
Wearing tight-fitting shoes
Wearing tight-fitting shoes can contribute to the development of foot fungus. Tight shoes can cause excessive sweating and restrict airflow, creating a damp and warm environment that promotes fungal growth. Choosing properly fitting shoes with adequate ventilation can reduce the risk of infection.
Weakened immune system
A weakened immune system can make individuals more susceptible to foot fungus. Conditions such as diabetes, HIV/AIDS, or certain medications that suppress the immune system can increase the risk of fungal infections. It is essential to manage any underlying health conditions and follow medical advice to help prevent foot fungus.
Prevention
Keep feet clean and dry
Maintaining good foot hygiene is crucial in preventing foot fungus. Wash your feet with soap and water regularly, particularly after activities that cause excessive sweating. Thoroughly dry your feet, paying attention to the spaces between your toes, to minimize moisture that can promote fungal growth.
Avoid walking barefoot in public areas
To reduce the risk of fungal infection, avoid walking barefoot in public areas such as locker rooms, swimming pool areas, or communal showers. Consider wearing protective footwear, such as flip-flops or sandals, to minimize direct contact with contaminated surfaces.

Use antifungal powders or sprays
Antifungal powders or sprays can be used as a preventive measure against foot fungus. These products can help reduce moisture and inhibit fungal growth. Apply them to your feet and inside your shoes, paying attention to areas prone to excessive sweating.
Wear breathable footwear
Proper footwear plays a significant role in preventing foot fungus. Choose shoes made of breathable materials such as leather or mesh, as they allow air circulation and help keep your feet dry. Avoid tight-fitting or non-breathable shoes that trap moisture and heat.
Change socks regularly
Wearing clean socks and changing them regularly can help prevent foot fungus. Opt for moisture-wicking socks that can draw away moisture from your feet. Avoid reusing dirty or damp socks as they can harbor fungi and contribute to infection.
Avoid sharing personal items
To minimize the risk of spreading and acquiring foot fungus, avoid sharing personal items such as socks, shoes, or towels. Fungi can survive on these items and transfer from one person to another. Use your own personal items to maintain proper hygiene.
Treatment
Topical antifungal creams or ointments
For mild cases of foot fungus, topical antifungal creams or ointments can often be an effective treatment. These products are applied directly to the affected area and help to eliminate the fungal infection. Follow the instructions provided by the healthcare professional or the product packaging for proper application.
Oral antifungal medications
In more severe or persistent cases of foot fungus, oral antifungal medications may be prescribed. These medications work from within the body to target the fungal infection. It is important to follow the recommended dosage and complete the full course of treatment to ensure the infection is completely cleared.
Home remedies like vinegar soaks
Some individuals find relief from foot fungus symptoms by using home remedies, such as vinegar soaks. Soaking the feet in a mixture of water and vinegar can help create an environment that is less favorable for fungal growth. Consult with a healthcare professional for guidance on specific home remedies and their effectiveness.
Keeping feet clean and dry
Proper foot hygiene is crucial in the treatment of foot fungus. Keeping the feet clean and dry can help prevent the spread of infection and promote healing. Regularly wash your feet with a mild soap and thoroughly dry them, paying attention to the areas between the toes.
Proper toenail care
For toenail fungus, proper toenail care is essential for treatment. Keep your nails trimmed and clean, and avoid wearing nail polish, as it can trap moisture and worsen the infection. If necessary, consult with a healthcare professional or a podiatrist for guidance on appropriate toenail care.
Seeking medical advice
If you suspect you have foot fungus or if your symptoms persist or worsen despite self-care measures, it is important to seek medical advice. A healthcare professional can accurately diagnose the type of foot fungus and recommend appropriate treatment options tailored to your specific condition. Human doctors and podiatrists have the expertise to provide guidance and prescribe medications if necessary.
In conclusion, foot fungus can have various appearances and symptoms depending on the type of infection. It is important to be aware of the signs of foot fungus, such as redness, itching, scaling, and changes in nail texture or color. Taking preventive measures, including maintaining good foot hygiene and avoiding walking barefoot in public areas, can help reduce the risk of fungal infections. If foot fungus does occur, there are treatment options available, ranging from topical creams to oral medications, that can effectively eliminate the infection.
Additional Resources

More and more Americans are finally getting rid of toenails fungus completely. They’re doing this thanks to an African tribe’s incredible and well-kept secret that is able to destroy any fungal infection.
The entire medical community is in utter shock because of it…
This video is going to show how simple it actually is to get rid of any contagious fungal infection fast and natural without any dangerous side effects.
The African trick is as cheap as it is simple and efficient, and no matter how yellow, itchy or smelly your toes are right now, it is guaranteed to easily flush away all the fungus in your body.
From this… To this…
This sacred African ritual which has been thoroughly studied and its beneficial effects have been confirmed by over a dozen independent sources, such as the The Journal of European Academy Of Dermatology or National Center for Biotechnology Information.