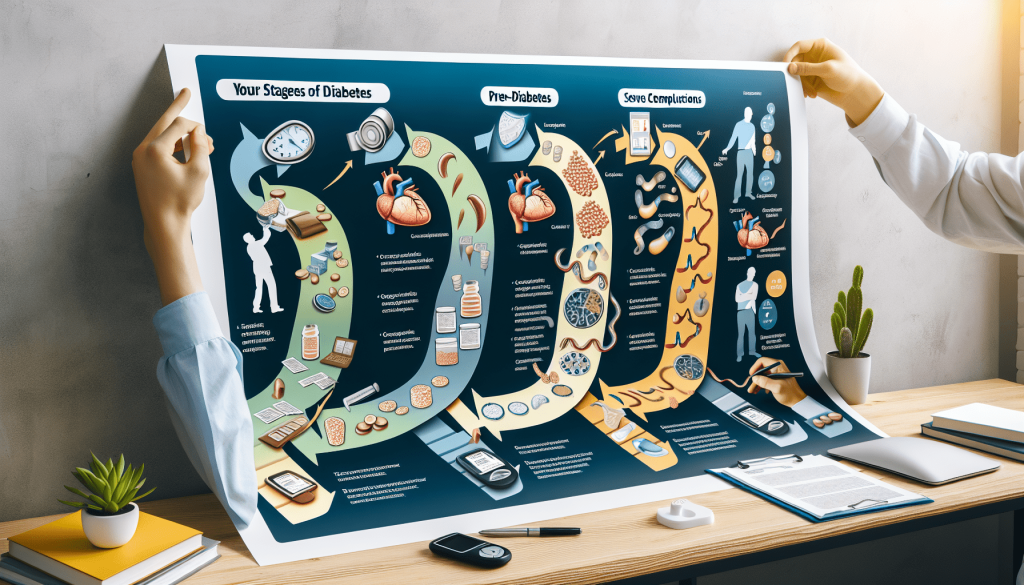
What Are The 4 Stages Of Diabetes?
In this article, we will explore the 4 stages of diabetes and how they affect your health. From pre-diabetes to the severe complications of advanced diabetes, understanding each stage can help you take control of your condition and make informed choices for your well-being. So, whether you’ve been recently diagnosed or have been living with diabetes for years, let’s take a friendly journey together and learn more about the unique stages of this metabolic disorder.
Prediabetes
Definition and Criteria
Prediabetes is a condition in which your blood sugar levels are higher than normal, but not high enough to be diagnosed as type 2 diabetes. It is considered a warning sign that you are at risk for developing full-blown diabetes in the future. The criteria for diagnosing prediabetes include a fasting blood glucose level between 100 and 125 mg/dL, an oral glucose tolerance test result between 140 and 199 mg/dL, or a hemoglobin A1c level between 5.7% and 6.4%.
Symptoms
Unlike type 1 or type 2 diabetes, prediabetes does not usually cause any noticeable symptoms. However, some individuals may experience subtle signs such as increased thirst, frequent urination, unexplained weight loss, or fatigue. These symptoms are often mild and can easily be attributed to other factors, making them easy to overlook.
Diagnosis
Prediabetes is diagnosed through blood tests that measure your blood sugar levels. The most common tests include a fasting plasma glucose (FPG) test, an oral glucose tolerance test (OGTT), and a hemoglobin A1c (HbA1c) test. These tests help determine how well your body is able to regulate your blood sugar levels and assess if you are at risk for developing diabetes. It is recommended that adults should be tested for prediabetes at least every three years starting at age 45, or sooner if they have certain risk factors such as being overweight or having a family history of diabetes.
Prevention and Management
If you are diagnosed with prediabetes, it is important to take action to prevent or delay the onset of type 2 diabetes. The good news is that with lifestyle changes, prediabetes can often be reversed. Losing just 5-7% of your body weight through a combination of healthy eating and regular physical activity can greatly reduce your risk. It is also important to make healthy food choices, limit your intake of sugary beverages, and incorporate regular exercise into your daily routine. In some cases, your healthcare provider may prescribe medication to help manage your blood sugar levels and reduce your risk of developing diabetes.
Type 1 Diabetes
Definition and Causes
Type 1 diabetes, also known as insulin-dependent diabetes or juvenile diabetes, is a chronic condition in which the pancreas produces little to no insulin. Insulin is a hormone that allows glucose to enter your cells and provide them with energy. The exact cause of type 1 diabetes is unknown, but it is thought to be an autoimmune disease, where the body mistakenly attacks and destroys the insulin-producing cells in the pancreas. This results in a lifelong dependence on insulin injections or the use of an insulin pump to manage blood sugar levels.
Symptoms
The symptoms of type 1 diabetes typically develop rapidly and can include increased thirst, frequent urination, extreme hunger, unexplained weight loss, fatigue, irritability, blurred vision, and slow-healing sores or infections. These symptoms occur because without insulin, your body cannot effectively use the glucose from food as fuel. Instead, it begins to break down fat for energy, producing ketones as a byproduct. This can lead to a potentially life-threatening condition called diabetic ketoacidosis (DKA), which requires immediate medical attention.
Diagnosis
Type 1 diabetes is diagnosed through blood tests that measure your blood sugar levels and the presence of autoantibodies. The most common tests include a fasting blood glucose test, an oral glucose tolerance test, and a glycated hemoglobin (HbA1c) test. Additionally, the presence of specific autoantibodies, such as islet cell antibodies (ICA), glutamic acid decarboxylase autoantibodies (GADA), and insulin autoantibodies (IAA), can help confirm the diagnosis. It is crucial to get an accurate diagnosis and start treatment as soon as possible to prevent complications associated with uncontrolled high blood sugar levels.
Treatment
The main treatment for type 1 diabetes is insulin therapy. Insulin is typically administered through multiple daily injections or by using an insulin pump. The goal of insulin therapy is to mimic the body’s natural insulin production and maintain blood sugar levels within a target range. In addition to insulin therapy, managing type 1 diabetes involves regular blood sugar monitoring, a healthy diet, regular physical activity, and maintaining a healthy weight. Education and support from healthcare professionals, as well as the adoption of a structured diabetes management plan, are crucial for successfully managing type 1 diabetes.

Type 2 Diabetes
Definition and Causes
Type 2 diabetes, also known as adult-onset diabetes, is a chronic condition that affects the way your body metabolizes sugar (glucose). It occurs when your body becomes resistant to the effects of insulin or when your pancreas does not produce enough insulin to maintain normal blood sugar levels. The exact cause of type 2 diabetes is multifactorial and involves a combination of genetic and lifestyle factors, including being overweight or obese, having a sedentary lifestyle, having a family history of diabetes, and certain ethnic backgrounds (such as African, Hispanic, or Asian descent).
Symptoms
The symptoms of type 2 diabetes develop gradually and may be mild at first. Common symptoms include increased thirst, frequent urination, fatigue, blurred vision, slow-healing wounds, recurrent infections, and darkened patches of skin. Many individuals with type 2 diabetes may not experience any noticeable symptoms, which is why the condition often goes undiagnosed for years. Regular check-ups and blood tests are essential for early detection and management of type 2 diabetes.
Diagnosis
Type 2 diabetes is diagnosed through various blood tests that measure your blood sugar levels. The most common tests include fasting plasma glucose (FPG) and oral glucose tolerance test (OGTT). These tests help determine how well your body is regulating glucose and can identify if you have high blood sugar levels indicative of diabetes. Additionally, a glycated hemoglobin (HbA1c) test can provide an overview of your average blood sugar levels over the past few months. It is important to get screened for diabetes regularly, especially if you have risk factors such as being overweight, having a sedentary lifestyle, or a family history of diabetes.
Treatment
The treatment for type 2 diabetes focuses on managing blood sugar levels through lifestyle changes, medication, and, in some cases, insulin therapy. Lifestyle modifications, including adopting a healthy diet, engaging in regular physical activity, achieving and maintaining a healthy weight, and avoiding tobacco and excessive alcohol consumption, are essential for managing type 2 diabetes. Oral medications, such as metformin, and injectable medications, like glucagon-like peptide-1 (GLP-1) receptor agonists and sodium-glucose cotransporter-2 (SGLT-2) inhibitors, may be prescribed to help improve insulin sensitivity and regulate blood sugar levels. In more advanced cases, insulin injections or pump therapy may be necessary to maintain optimal blood sugar control.
Gestational Diabetes
Definition and Causes
Gestational diabetes is a form of diabetes that occurs during pregnancy. It is characterized by high blood sugar levels that develop during pregnancy and usually resolve after childbirth. The exact cause of gestational diabetes is not fully understood, but it is believed to be related to hormonal changes that occur during pregnancy. The hormones produced by the placenta can impair the action of insulin in the mother’s body, resulting in elevated blood sugar levels.
Symptoms
Gestational diabetes often does not present with noticeable symptoms, which is why routine screening during pregnancy is crucial for early detection. However, some women may experience increased thirst, frequent urination, fatigue, or blurred vision. These symptoms are often mild and can be mistaken for normal pregnancy discomforts. It is important to attend regular prenatal check-ups and undergo the recommended gestational diabetes screening tests to ensure the health of both the mother and the baby.
Diagnosis
Gestational diabetes is diagnosed through an oral glucose tolerance test (OGTT) performed between weeks 24 and 28 of pregnancy. During the test, you will be asked to drink a sugary beverage, and your blood sugar levels will be measured at specific intervals. If your blood sugar levels are higher than normal at any point during the test, you will be diagnosed with gestational diabetes. It is essential to diagnose and manage gestational diabetes promptly to prevent complications for both the mother and the baby.
Treatment
The main treatment for gestational diabetes involves lifestyle modifications, such as following a balanced diet, engaging in regular physical activity, and monitoring blood sugar levels. In some cases, insulin therapy or other diabetes medications may be necessary to achieve optimal blood sugar control. Regular check-ups with healthcare professionals and close monitoring of blood sugar levels are essential throughout the pregnancy to ensure the health and well-being of both the mother and the baby. After delivery, blood sugar levels usually return to normal, but women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life. Therefore, regular follow-up and ongoing diabetes screening are recommended.
Additional Resources

If you’ve been battling high blood sugar and diet & exercise haven’t yielded the results you hoped for…
A prominent medical expert has uncovered an extraordinary breakthrough that you need to know about.
Participants in a recent double-blind study who tried this special combination of ingredients… Not only witnessed significant improvements in insulin sensitivity… But also achieved well-regulated blood sugar levels.
In addition, they managed to lose an average of 27 lbs. during the experiment.
Imagine simply incorporating this unique blend of ingredients into your breakfast or dinner… And effectively managing your blood sugar levels – without restrictive diets, grueling workouts, or dubious medications.