Is Neuropathy Life Threatening?
Living with neuropathy can be a challenging experience, but understanding its potential risks and impact on your overall health is vital. In this article, we will explore whether neuropathy is a life-threatening condition or not. We’ll delve into the various types of neuropathy, discuss its symptoms and causes, and discover the potential complications it might pose. By the end, you’ll have a clearer understanding of how neuropathy affects your well-being and whether it requires immediate medical attention. So, let’s dive into this informative journey together and uncover the truth about neuropathy’s life-threatening nature.
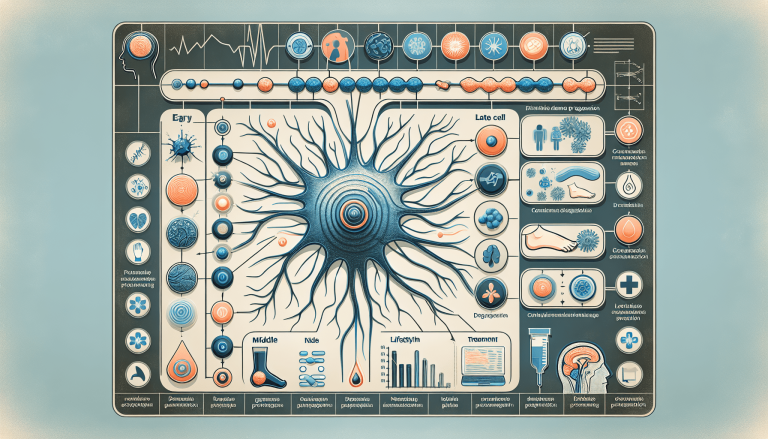
Understanding Neuropathy
Definition of neuropathy
Neuropathy, also known as peripheral neuropathy, is a condition that affects the peripheral nerves, which connect the brain and spinal cord to the rest of the body. These nerves are responsible for transmitting signals to and from different parts of the body, allowing us to move, feel sensations, and control bodily functions. When these nerves are damaged or disrupted, it can lead to a wide range of symptoms and complications.
Causes of neuropathy
Neuropathy can have various causes, including chronic diseases such as diabetes, autoimmune disorders, infections, trauma or injuries, exposure to toxins, certain medications, and hereditary factors. In some cases, the exact cause may remain unknown. Understanding the underlying cause is important in determining the appropriate treatment and management strategies.
Types of neuropathy
There are different types of neuropathy, each with its own set of symptoms and affected nerves. Some common types include diabetic neuropathy, which is associated with diabetes; peripheral neuropathy, which affects the limbs; autonomic neuropathy, which affects the nerves controlling involuntary bodily functions; and focal neuropathy, which causes damage to a specific nerve or group of nerves. It is essential to identify the type of neuropathy to tailor treatment plans accordingly.
Symptoms of neuropathy
The symptoms of neuropathy can vary depending on the type and severity of the condition. Common symptoms include numbness or tingling in the hands and feet, sharp or burning pain, muscle weakness, sensitivity to touch, loss of coordination, and impaired balance. Some individuals may also experience changes in temperature and sweating patterns, as well as digestive and bladder problems. Recognizing these symptoms is crucial for early diagnosis and intervention.
Effects and Complications of Neuropathy
Impact on daily life
Neuropathy can significantly impact daily life, making simple tasks challenging and affecting overall quality of life. The numbness and tingling sensations can limit your ability to grip objects, button clothes, or perform other fine motor activities. Muscle weakness and coordination issues can make walking, climbing stairs, and maintaining balance difficult. Additionally, the pain associated with neuropathy can be debilitating and affect sleep, concentration, and mood.
Physical complications
In addition to the impact on daily life, neuropathy can lead to various physical complications. For example, decreased sensation in the feet can increase the risk of developing foot ulcers or injuries that go unnoticed. The weakened muscles and impaired balance can also elevate the risk of falls and fractures. Furthermore, changes in blood circulation can result in skin infections and delayed wound healing.
Emotional and psychological effects
Living with neuropathy can take a toll on your emotional and psychological well-being. The chronic pain and discomfort can lead to anxiety, depression, and frustration. The gradual loss of independence and reliance on others for assistance with daily activities can also contribute to feelings of helplessness and low self-esteem. It is important to address these emotional and psychological effects alongside the physical symptoms of neuropathy.
Risk of falls and injuries
Neuropathy increases the risk of falls and injuries due to the loss of sensation and compromised balance. Falls can result in fractures, head injuries, and other serious consequences, particularly in older adults. It is essential to take necessary precautions, such as removing tripping hazards, using assistive devices like canes or walkers, and practicing exercises to improve balance and strength.

Severity of Neuropathy
Different levels of severity
Neuropathy can range from mild to severe, depending on the extent of nerve damage. The severity of neuropathy can impact the symptoms experienced by an individual, as well as the overall prognosis and treatment options. Understanding the severity level is essential in formulating an appropriate management plan.
Mild neuropathy
In cases of mild neuropathy, individuals may experience occasional or mild symptoms that do not significantly interfere with daily activities. The symptoms may be intermittent and may not require medical intervention. However, it is important to monitor the progression of the condition, as mild neuropathy can worsen over time if left untreated.
Moderate neuropathy
Moderate neuropathy is characterized by more frequent and noticeable symptoms that can disrupt daily life to a greater extent. The pain and sensory changes may lead to limitations in physical activities and a decrease in functional independence. Medical intervention and treatment strategies are generally recommended to manage the symptoms and prevent further progression.
Severe neuropathy
Severe neuropathy is associated with persistent and debilitating symptoms that severely impact daily functioning and overall quality of life. The pain, muscle weakness, and loss of coordination can make it challenging to carry out even basic activities. Treatment approaches become more aggressive in severe cases, aiming to alleviate pain, improve function, and prevent further deterioration.
Life-Threatening Conditions Associated with Neuropathy
Autonomic neuropathy complications
Autonomic neuropathy, a type of neuropathy affecting the nerves controlling involuntary bodily functions, can lead to life-threatening complications. These complications may include disruptions in heart rate and blood pressure regulation, digestion problems, bladder and bowel dysfunction, and sexual dysfunction. Effective management and monitoring of autonomic neuropathy are crucial to reduce the risk of serious complications.
Neuropathy and cardiovascular health
Neuropathy can have a significant impact on cardiovascular health. The damage to the nerves controlling heart rate and blood vessels can contribute to abnormal heart rhythms, irregular blood pressure, and reduced blood flow to vital organs. These factors increase the risk of heart disease, heart attacks, strokes, and other cardiovascular complications. Regular monitoring and appropriate treatment are essential for maintaining cardiovascular health in individuals with neuropathy.
Increased risk of infections
Neuropathy can weaken the immune system, making individuals more susceptible to infections. Common infections associated with neuropathy include urinary tract infections, skin infections, and respiratory tract infections. Prompt identification and treatment of infections, along with preventive measures, are crucial to minimize the risk of complications.
Impact on respiratory function
In some cases, neuropathy can affect the nerves responsible for controlling the respiratory muscles, leading to breathing difficulties and compromised lung function. This can result in reduced oxygen levels and increased susceptibility to respiratory infections. Regular monitoring of respiratory function, along with targeted interventions, can help manage these complications and optimize respiratory health.

Managing and Treating Neuropathy
Lifestyle changes
Lifestyle modifications play a key role in managing neuropathy and reducing its impact on daily life. These may include maintaining a healthy diet to support nerve health, managing blood sugar levels for individuals with diabetic neuropathy, quitting smoking and limiting alcohol consumption to improve overall circulation, practicing regular exercise to improve muscle strength and balance, and managing stress levels to alleviate the pain and discomfort associated with neuropathy.
Medications for neuropathy
Various medications can be prescribed to address the symptoms and complications of neuropathy. These may include pain relievers such as over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), prescription medications like gabapentin or pregabalin that target nerve pain specifically, and antidepressants or anticonvulsant medications that can help modulate pain signals. Medications should be used under the guidance of a healthcare professional to ensure appropriate dosing and monitor for potential side effects.
Physical therapy and exercises
Physical therapy and exercises play an important role in managing neuropathy and improving function. Physical therapists can design exercise programs to improve strength, balance, and coordination, which can reduce the risk of falls and improve mobility. Additionally, therapies such as massage, heat therapy, and occupational therapy may be employed to alleviate pain, improve circulation, and enhance daily functioning.
Alternative and complementary therapies
Complementary and alternative therapies may be considered as adjunct treatments for neuropathy. These include acupuncture, transcutaneous electrical nerve stimulation (TENS), herbal supplements, and dietary modifications. While some individuals may experience relief from these therapies, it is important to discuss their use with a healthcare professional to ensure their safety and effectiveness.
Prevention and Risk Reduction
Taking care of underlying conditions
Identifying and managing underlying conditions that can contribute to neuropathy is essential for prevention and risk reduction. For individuals with diabetes, maintaining optimal blood sugar control is crucial in preventing further nerve damage. Other conditions such as autoimmune disorders should be treated and managed effectively to minimize the risk of neuropathy and its complications.
Healthy lifestyle choices
Adopting a healthy lifestyle can significantly reduce the risk of developing neuropathy. This includes eating a balanced diet rich in antioxidants and essential nutrients, engaging in regular physical activity, maintaining a healthy weight, avoiding smoking and excessive alcohol consumption, and managing stress levels. These lifestyle choices promote overall nerve health and reduce the risk of neuropathy.

Regular monitoring and check-ups
Regular check-ups with healthcare professionals are important for individuals with existing neuropathy or those at risk of developing it. These check-ups can help monitor the progression of the condition, assess the effectiveness of treatment plans, and identify any potential complications early on. Regular monitoring allows for timely interventions and adjustments in the treatment approach, optimizing overall outcomes.
Safety measures to prevent falls
Taking safety measures to prevent falls is crucial for individuals with neuropathy, particularly those with balance and coordination issues. Simple steps can be taken, such as removing clutter and tripping hazards from the living environment, installing grab bars and handrails, ensuring adequate lighting, and wearing appropriate footwear. These precautions can significantly reduce the risk of falls and related injuries.
Implications for Quality of Life
Challenges in daily activities
Neuropathy can present numerous challenges in daily activities. Simple tasks such as buttoning clothes, holding utensils, or picking up objects can become difficult due to numbness and weakness in the hands. Walking, performing household chores, and participating in recreational activities may also be hindered by balance and coordination issues. Recognizing these challenges and seeking appropriate support and accommodations can help mitigate their impact.
Impact on independence
The gradual progression of neuropathy and the associated complications can impact independence. Individuals may become reliant on others for assistance with daily activities, transportation, and personal care. This loss of independence can lead to frustration, decreased self-esteem, and changes in social dynamics. It is important to explore strategies and resources that promote independence and maintain a sense of control.
Financial burden
Neuropathy can impose a significant financial burden on individuals and their families. The costs associated with medical consultations, diagnostic tests, medications, assistive devices, and therapy sessions can add up over time. Moreover, the impact on work productivity and potential loss of income due to limited physical capabilities can further exacerbate the financial strain. Exploring insurance coverage and seeking financial assistance programs may help alleviate this burden.
Social and emotional support
Living with neuropathy can be emotionally challenging, and having a strong support system is crucial. Family, friends, and support groups can provide emotional support, understanding, and encouragement during difficult times. Counseling or therapy sessions may also be beneficial in helping individuals cope with the emotional and psychological effects of neuropathy. Seeking out these resources and building a network of support can significantly improve the quality of life for individuals with neuropathy.
Prognosis and Long-Term Outlook
Progression of neuropathy
The progression of neuropathy can vary from person to person and depends on several factors, including the underlying cause, severity, and individual response to treatment. In some cases, neuropathy may stabilize or even improve with effective management strategies. However, for others, the condition may continue to progress over time, leading to more severe symptoms and complications if left untreated.
Factors influencing prognosis
Several factors can influence the prognosis of neuropathy. Timely diagnosis and early intervention play a crucial role in managing the condition and preventing further nerve damage. Compliance with treatment plans, lifestyle modifications, and adherence to medications can also impact the prognosis. Additionally, the presence of other underlying medical conditions and the individual’s overall health can influence the long-term outlook of neuropathy.
Treatment effectiveness
The effectiveness of treatment approaches for neuropathy varies depending on the individual’s specific circumstances. While some individuals may experience significant relief from symptoms and improved function with treatment, others may have a more modest response or require ongoing symptom management. It is important to work closely with healthcare professionals to find the most effective treatment plan for each individual case.
Coping strategies
Coping with neuropathy requires a multifaceted approach. Engaging in self-care practices, such as following a healthy diet, engaging in regular physical activity, and practicing stress management techniques, can help individuals cope with the challenges of neuropathy. Support from healthcare professionals, therapists, and support groups can provide guidance, education, and emotional support. Developing effective coping strategies tailored to individual needs is crucial in managing the physical and emotional aspects of neuropathy.
Seeking Professional Help
Importance of medical advice
Seeking medical advice is crucial when dealing with neuropathy. Professionals specializing in neurology and related fields are equipped with the knowledge and expertise to accurately diagnose and manage neuropathy. They can conduct comprehensive evaluations, order relevant tests and imaging, prescribe appropriate medications, and develop personalized treatment plans. Prompt medical attention ensures early intervention and reduces the risk of complications.
Neuropathy specialists
Neuropathy specialists play a key role in the diagnosis and management of neuropathy. Neurologists, in particular, are trained to evaluate and treat conditions affecting the nervous system, including neuropathy. They can provide specialized expertise and access to the latest research and treatment options. In complex cases or cases with specific types of neuropathy, seeking a consultation with a neuropathy specialist can provide tailored care and improve outcomes.
Support from healthcare professionals
In addition to neuropathy specialists, various healthcare professionals can contribute to the comprehensive management of neuropathy. Physiotherapists, occupational therapists, pain management specialists, and nurses familiar with neuropathy can provide valuable support and guidance. Collaborating with a multidisciplinary team ensures a holistic approach to addressing the symptoms and complications of neuropathy.

Accessing appropriate resources
Finding appropriate resources and support is an important aspect of managing neuropathy. Reliable sources of information, educational materials, and support networks can empower individuals with knowledge and connect them with others experiencing similar challenges. Organizations specializing in neuropathy, online forums, and local support groups can provide a wealth of information and support.
Conclusion
Importance of understanding neuropathy
Understanding neuropathy is essential for individuals living with the condition, their loved ones, and healthcare professionals. By increasing awareness and knowledge about neuropathy, individuals can recognize the symptoms, seek early diagnosis and intervention, and actively participate in their own care. Healthcare professionals can benefit from comprehensive understanding to provide optimal care and support.
Awareness and education
Raising awareness about neuropathy can help dispel misconceptions and reduce stigma associated with the condition. Educating individuals about the causes, symptoms, and treatment options enables proactive management and empowers those affected by neuropathy to seek appropriate support and resources. Furthermore, increased awareness can facilitate early detection and intervention, potentially preventing the progression of neuropathy and its associated complications.
Promoting early detection and treatment
Early detection and treatment are essential in effectively managing neuropathy. By recognizing the early symptoms and seeking medical advice promptly, individuals have a better chance of receiving appropriate interventions to alleviate pain, manage symptoms, and minimize complications. Regular check-ups and monitoring can enable timely adjustments to treatment plans and ensure the best possible outcomes.
Improving quality of life
The impact of neuropathy on quality of life can be significant, but with the right management strategies and support, individuals can regain control and enhance their overall well-being. Accessing appropriate treatments, implementing lifestyle changes, seeking emotional support, and adopting coping strategies can help individuals navigate the challenges of neuropathy and improve their quality of life.
In conclusion, neuropathy is a complex condition that can have a profound impact on various aspects of a person’s life. Understanding the causes, symptoms, and complications of neuropathy is crucial for individuals, their loved ones, and healthcare professionals. By promoting awareness, encouraging early detection and treatment, and providing comprehensive support, the prognosis and quality of life for individuals living with neuropathy can be significantly improved.
Additional Resources

| According to a leading research hospital, a simple 3-ingredient “cocktail” may be able to not only reduce symptoms of nerve damage… but in some cases undo the damage done by nerve pain…Whether you’ve had the disease for 5, 10, or even 15 years.
Study after study has come out supporting the power of these vitamins against damaged nerve cells. And what’s more amazing… is that when taken together, these ingredients have helped people see partial or total elimination of their symptoms in a matter of days. Without changes to their diet… without taking prescription medications… and without even exercising… |