How Fast Does Neuropathy Progress?
Neuropathy, a condition that affects the nerves, can be a cause of concern for many individuals. If you’ve recently been diagnosed with neuropathy or know someone who has, you may be wondering about the speed at which this condition progresses. Understanding the progression of neuropathy is vital in managing its symptoms and seeking appropriate treatment. In this article, we will explore the rate at which neuropathy progresses, shedding light on this common question and providing you with valuable information for your journey ahead.
Understanding Neuropathy
Neuropathy is a medical condition that affects the nerves, causing damage and dysfunction. It is characterized by pain, tingling, numbness, and weakness in the affected areas. To truly understand neuropathy, let’s dive into its definition, causes, and symptoms.
Definition of neuropathy
Neuropathy, also known as peripheral neuropathy, is a condition that occurs when the peripheral nerves, which connect the brain and spinal cord to the rest of the body, become damaged. This can lead to various symptoms, depending on which nerves are affected. Neuropathy can be caused by a variety of factors, including underlying diseases, injuries, and genetic predisposition.
Causes of neuropathy
There are various causes of neuropathy, and understanding them can help in identifying and managing the condition. Common causes include diabetes, autoimmune diseases, infections, exposure to toxins, vitamin deficiencies, and certain medications. Nerve damage can also occur as a result of physical trauma, such as injuries or accidents.
Symptoms of neuropathy
Neuropathy manifests through a range of symptoms, which can vary depending on the type and severity of the condition. Common symptoms include pain, numbness, tingling (often described as pins and needles), muscle weakness, and a loss of coordination. Individuals with neuropathy may also experience changes in their sense of touch, temperature sensitivity, and reflexes.
Types of Neuropathy
Neuropathy can present itself in different ways, affecting different types of nerves in the body. This leads to distinct types of neuropathy, including peripheral neuropathy, diabetic neuropathy, autonomic neuropathy, and cranial neuropathy.
Peripheral neuropathy
Peripheral neuropathy is the most common type of neuropathy and typically affects the hands, feet, arms, and legs. It can cause pain, numbness, and a loss of sensation in these areas. Peripheral neuropathy can have various underlying causes, such as diabetes or nerve damage from injuries.
Diabetic neuropathy
Diabetic neuropathy is a specific type of neuropathy that occurs in individuals with diabetes. High blood sugar levels, along with other factors related to the disease, can damage the nerves over time. Diabetic neuropathy often affects the legs and feet and can cause pain, numbness, and a heightened risk of foot ulcers or infections.
Autonomic neuropathy
Autonomic neuropathy affects the autonomic nervous system, which is responsible for regulating various involuntary functions in the body, such as heart rate, digestion, and respiratory function. Symptoms of autonomic neuropathy can include gastrointestinal issues, cardiovascular problems, sexual dysfunction, and erratic blood pressure.
Cranial neuropathy
Cranial neuropathy involves the nerves that control the senses and functions of the head and face. It can result in facial weakness, double vision, difficulty swallowing or speaking, and changes in taste or hearing. Cranial neuropathy can be caused by infections, inflammation, or other underlying medical conditions.
Factors Affecting Progression
The progression of neuropathy can vary from person to person, and several factors can influence how the condition develops over time. Understanding these factors is essential in managing and predicting the course of neuropathy.
Underlying cause of neuropathy
The underlying cause of neuropathy plays a significant role in its progression. If the cause can be effectively treated or managed, the neuropathy may either stabilize or even improve. However, if the cause is chronic or progressive, the neuropathy may worsen over time.
Treatment and management
The treatment and management of neuropathy can also impact its progression. Early intervention, proper medical care, and adherence to recommended treatments can help slow down the advancement of the condition. Close monitoring, medication adjustments, and lifestyle modifications play crucial roles in managing neuropathy.
Individual’s overall health
An individual’s overall health can influence how neuropathy progresses. Maintaining good overall health, including a balanced diet, regular exercise, and healthy lifestyle choices, can positively impact the progression of neuropathy. Conversely, poor health habits or the presence of other medical conditions may exacerbate neuropathy symptoms.
Genetic factors
Genetic factors can contribute to the progression of neuropathy. Some individuals may have an inherited predisposition to developing neuropathy or may be more susceptible to certain types of neuropathies. Genetic testing can help identify these factors and guide treatment planning.
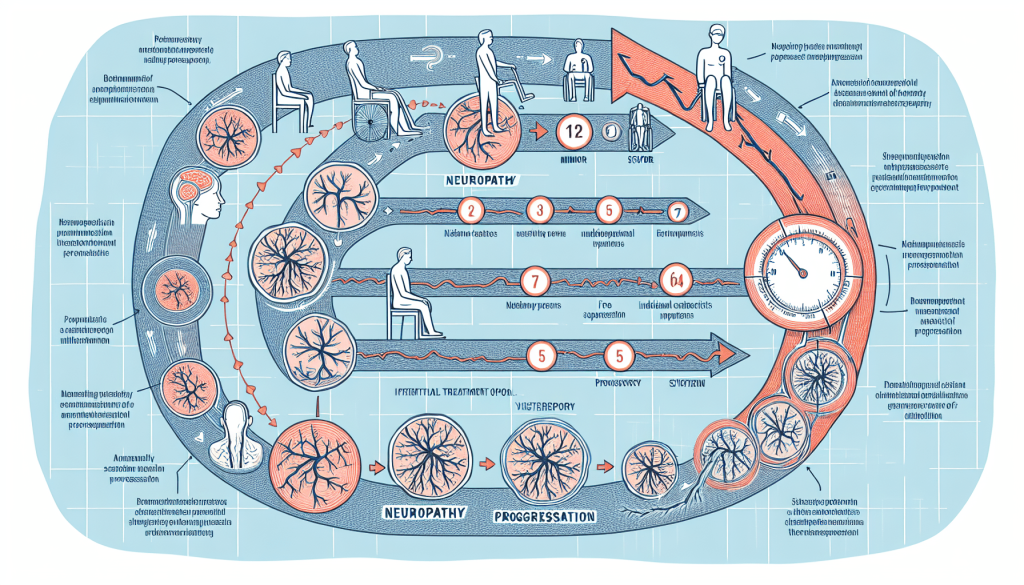
Progression Patterns
Neuropathy can progress at varying rates, depending on several factors. Understanding the different progression patterns can provide insights into the possible course of the condition.
Varied progression rates
Neuropathy progression rates can vary widely from person to person. Some individuals may experience a gradual progression over many years, while others may have a more rapid decline. The specific type of neuropathy, its underlying cause, and individual factors all contribute to the rate at which neuropathy progresses.
Rapid progression
In certain cases, neuropathy can progress rapidly, leading to severe symptoms and functional impairment. This can occur when the underlying cause of neuropathy is aggressive, involves widespread nerve damage, or is difficult to manage effectively. Prompt diagnosis and appropriate treatment are crucial in minimizing the impact of rapid progression.
Slow progression
On the other hand, neuropathy may progress slowly in some individuals. This can be the case when the underlying cause is well-managed, the nerve damage is relatively mild, or the individual responds well to treatment. Regular monitoring and appropriate interventions are still necessary to prevent further deterioration and manage symptoms effectively.
Stages of neuropathy progression
Neuropathy progression can be categorized into different stages based on the severity of symptoms and functional limitations. These stages help healthcare professionals track the progression, assess the treatment response, and plan interventions accordingly. The stages can range from mild and early symptoms to severe complications that significantly impact an individual’s quality of life.
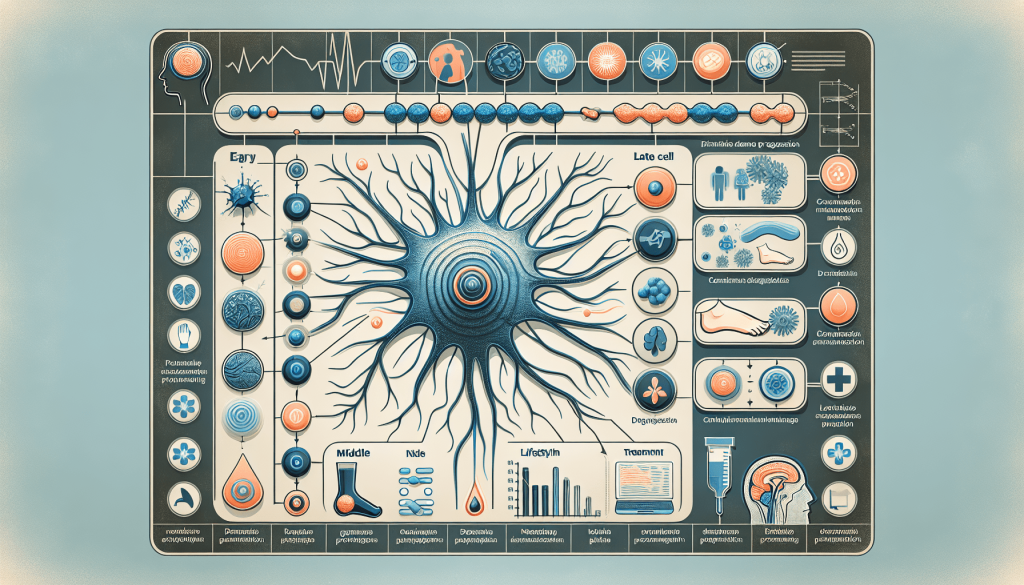
Common Symptoms of Progression
As neuropathy progresses, certain symptoms may become more pronounced or new symptoms may develop. Recognizing these common symptoms can help individuals and healthcare professionals identify the progression of neuropathy and adjust treatment strategies accordingly.
Increase in pain intensity
One of the hallmark symptoms of neuropathy progression is an increase in pain intensity. The pain may become more frequent, severe, or spread to new areas as the condition worsens. Effective pain management strategies become increasingly important in providing relief and improving quality of life.
Worsening tingling and numbness
The tingling and numbness associated with neuropathy can intensify as the condition progresses. These sensations may extend to larger areas or become more persistent, leading to greater discomfort and functional limitations. Addressing these symptoms through medication adjustments or lifestyle modifications is crucial.
Muscle weakness
Neuropathy can cause muscle weakness as the nerves responsible for muscle control become damaged. This weakness can affect specific muscle groups or be more generalized, impacting overall mobility and coordination. Physical therapy and regular exercise can help maintain muscle strength and improve functional abilities.
Loss of coordination
Loss of coordination is a common symptom of advanced neuropathy. The damaged nerves make it challenging for the brain to communicate effectively with the muscles, leading to unsteadiness, imbalance, and difficulty with fine motor skills. Assistive devices and occupational therapy may be beneficial in managing coordination issues.
Diagnosing and Monitoring Progression
To effectively manage neuropathy and track its progression, healthcare professionals rely on a combination of diagnostic tools and monitoring methods. These allow for a comprehensive assessment of the condition and inform the development of personalized treatment plans.
Medical history and physical examination
A thorough medical history review, including a detailed account of symptoms, their progression, and any relevant past medical conditions or injuries, is essential in diagnosing neuropathy. A physical examination can help evaluate neurological function, assess muscle strength and coordination, and identify any visible signs of nerve damage.

Electromyography (EMG) and nerve conduction studies
Electromyography (EMG) and nerve conduction studies are commonly used tests to assess the health and functioning of nerves and muscles. EMG involves inserting tiny needles into specific muscles to measure electrical activity, while nerve conduction studies evaluate how quickly signals travel along the nerves. These tests can help identify any abnormalities or damage to nerve fibers.
Blood tests
Blood tests are often conducted to rule out underlying medical conditions that can lead to neuropathy, such as diabetes, vitamin deficiencies, kidney or liver dysfunction, or autoimmune diseases. Blood tests can also measure glucose levels, electrolyte imbalances, and markers of inflammation, providing valuable insights into the overall health of an individual.
Quantitative sensory testing
Quantitative sensory testing is a specialized evaluation that assesses various aspects of sensory perception, such as touch, temperature, and vibration. It can identify changes in sensory thresholds and different types of nerve damage. This testing helps further characterize the extent and progression of neuropathy.
Preventing or Slowing Progression
While neuropathy may not be completely curable, there are measures individuals can take to prevent or slow down its progression. By addressing the underlying cause, maintaining good blood sugar control, making lifestyle modifications, and engaging in regular exercise, individuals can improve their quality of life and potentially slow the advancement of neuropathy.
Managing underlying cause
If neuropathy is caused by an underlying medical condition, effective management of that condition is crucial in preventing further nerve damage. Treating diabetes, managing autoimmune disorders, or avoiding exposure to toxins can significantly impact the progression of neuropathy.
Maintaining good blood sugar control
In the case of diabetic neuropathy, maintaining good blood sugar control is essential. Regular monitoring of blood glucose levels, adherence to medication or insulin regimens, and a healthy diet can help prevent further nerve damage and slow down the progression of neuropathy.
Lifestyle modifications
Adopting a healthy lifestyle can contribute to slowing the progression of neuropathy. This includes a balanced diet that provides essential nutrients, avoiding alcohol and smoking, managing stress, and avoiding repetitive motions or activities that can put excessive pressure on the nerves. Lifestyle modifications can help improve overall well-being and potentially slow neuropathy progression.
Regular exercise
Regular exercise, under the guidance of a healthcare professional, can be beneficial in managing neuropathy and preventing its progression. Exercise improves blood circulation, strengthens muscles, and enhances overall nerve function. Specific exercises and physical activities tailored to individual abilities and limitations can help alleviate symptoms and promote nerve health.
Treatment Options
Various treatment options are available to manage neuropathy and alleviate its symptoms. These options range from medications to physical therapy and complementary therapies.
Medications
Medications such as pain relievers, anti-seizure drugs, antidepressants, and topical creams may be prescribed to manage neuropathic pain and address specific symptoms. These medications work by targeting the underlying mechanisms of neuropathy and can provide significant relief.
Physical therapy
Physical therapy plays a crucial role in managing neuropathy by improving muscle strength, flexibility, and overall physical function. Physical therapists can design personalized exercise programs, provide manual therapy, and educate individuals on proper body mechanics, helping them manage neuropathy and reduce its impact on daily activities.

Transcutaneous electrical nerve stimulation (TENS)
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive therapy that involves applying low-level electrical currents to the skin, targeting specific nerves to alleviate pain and improve nerve function. TENS can be used as an at-home treatment option and offers a drug-free approach to managing neuropathic pain.
Complementary therapies
Complementary therapies, such as acupuncture, massage therapy, and relaxation techniques, may also provide symptom relief and improve overall well-being for individuals with neuropathy. These therapies can help reduce pain, improve circulation, and promote relaxation, enhancing the quality of life for those with neuropathy.
Complications of Neuropathy Progression
As neuropathy progresses, it can lead to various complications that further impact an individual’s quality of life. Recognizing and managing these complications is essential in providing comprehensive care.
Mobility issues
Neuropathy can cause significant mobility issues, making it challenging to perform daily tasks or participate in activities that were once enjoyable. Weakness, balance problems, and sensory disturbances can lead to falls, limitations in mobility, and a loss of independence. Assistive devices, physical therapy, and mobility aids can help mitigate these challenges.
Infections and ulcers
Neuropathy can limit sensation in the feet and hands, increasing the risk of injuries and the development of infections or ulcers. Poor wound healing and reduced immune function further contribute to this risk. Regular foot care, proper hygiene, and prompt treatment of any injuries or infections are critical to prevent complications.
Autonomic dysfunction
Autonomic neuropathy can lead to autonomic dysfunction, affecting various bodily functions. This dysfunction can lead to problems with digestion, blood pressure regulation, bladder function, and sexual dysfunction. Managing symptoms, making lifestyle modifications, and following medical recommendations help mitigate the impact of autonomic dysfunction.
Emotional and psychological impact
The progression of neuropathy can also have a significant emotional and psychological impact on individuals. Chronic pain, functional limitations, and the uncertainty of the condition’s course can lead to anxiety, depression, and a decreased quality of life. Support groups, counseling, and coping strategies can help individuals navigate these challenges and improve their emotional well-being.
Improving Quality of Life
While neuropathy may present challenges, there are strategies and interventions available to improve the quality of life for individuals living with the condition.
Pain management strategies
Managing neuropathic pain is crucial in enhancing quality of life. Combining medications, physical therapy, mindfulness techniques, and alternative pain relief options can provide significant relief and improve daily functioning. Working closely with healthcare professionals to find the most effective pain management strategies is essential.
Support groups and counseling
Support groups and counseling can provide individuals with neuropathy the opportunity to connect with others who understand their experiences. Sharing stories, seeking advice, and receiving emotional support from those facing similar challenges can be tremendously beneficial for coping with the condition and improving overall well-being.
Assistive devices
The use of assistive devices can help individuals with neuropathy regain or maintain their independence. Devices such as canes, walkers, or orthotic supports can assist with stability and mobility. Additionally, adaptive tools and equipment can assist with daily tasks such as dressing, cooking, or driving, minimizing the impact of neuropathy on daily life.
Alternative pain relief options
Alternative pain relief options, such as acupuncture, aromatherapy, or herbal remedies, may offer additional relief for individuals with neuropathy. These approaches can be used in conjunction with traditional treatments, under the guidance of healthcare professionals.
In conclusion, understanding neuropathy requires a comprehensive knowledge of its definition, causes, symptoms, and progression. By considering factors that affect its progression, recognizing common symptoms, and utilizing diagnostic tools, healthcare professionals can effectively diagnose and monitor neuropathy. Preventing or slowing its progression through managing underlying causes, maintaining good overall health, and adopting lifestyle modifications is crucial. Treatment options, along with managing complications, can improve the quality of life for individuals with neuropathy. With a combination of evidence-based interventions, support systems, and a proactive approach, individuals can navigate the challenges posed by neuropathy and improve their overall well-being.
Additional Resources

Harvard scientists have recently identified the real root cause of nerve pain.
And when you fix this… You can wave goodbye to the tingling, numbness and burning sensations in your hands and feet.
And you’ll no longer have to rely on medications, expensive creams, or compression socks…